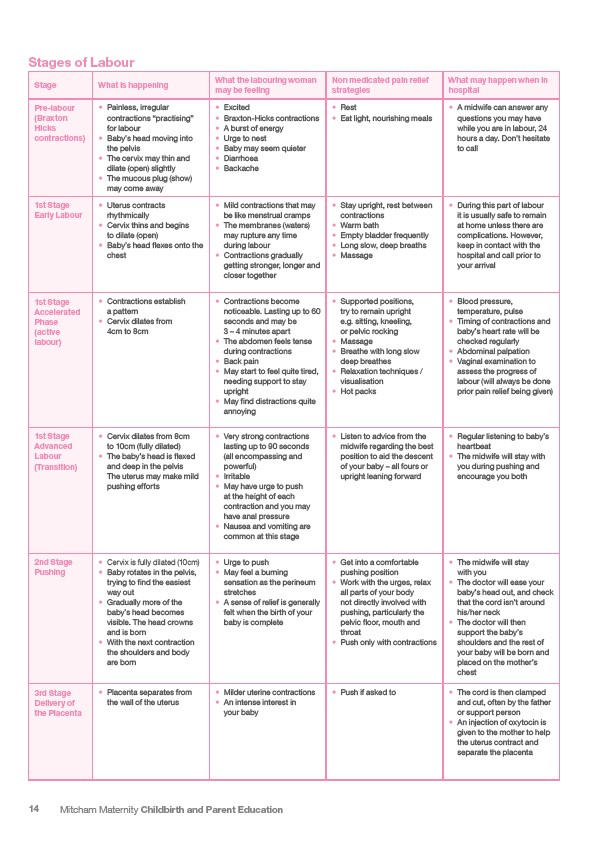
Stages of Labour
Stage What is happening
What the labouring woman
may be feeling
14 Mitcham Maternity Childbirth and Parent Education
Non medicated pain relief
strategies
What may happen when in
hospital
Pre-labour
(Braxton
Hicks
contractions)
• Painless, irregular
contractions “practising”
for labour
• Baby’s head moving into
the pelvis
• The cervix may thin and
dilate (open) slightly
• The mucous plug (show)
may come away
• Excited
• Braxton-Hicks contractions
• A burst of energy
• Urge to nest
• Baby may seem quieter
• Diarrhoea
• Backache
• Rest
• Eat light, nourishing meals
• A midwife can answer any
questions you may have
while you are in labour, 24
hours a day. Don’t hesitate
to call
1st Stage
Early Labour
• Uterus contracts
rhythmically
• Cervix thins and begins
to dilate (open)
• Baby’s head flexes onto the
chest
• Mild contractions that may
be like menstrual cramps
• The membranes (waters)
may rupture any time
during labour
• Contractions gradually
getting stronger, longer and
closer together
• Stay upright, rest between
contractions
• Warm bath
• Empty bladder frequently
• Long slow, deep breaths
• Massage
• During this part of labour
it is usually safe to remain
at home unless there are
complications. However,
keep in contact with the
hospital and call prior to
your arrival
1st Stage
Accelerated
Phase
(active
labour)
• Contractions establish
a pattern
• Cervix dilates from
4cm to 8cm
• Contractions become
noticeable. Lasting up to 60
seconds and may be
3 – 4 minutes apart
• The abdomen feels tense
during contractions
• Back pain
• May start to feel quite tired,
needing support to stay
upright
• May find distractions quite
annoying
• Supported positions,
try to remain upright
e.g. sitting, kneeling,
or pelvic rocking
• Massage
• Breathe with long slow
deep breathes
• Relaxation techniques /
visualisation
• Hot packs
• Blood pressure,
temperature, pulse
• Timing of contractions and
baby’s heart rate will be
checked regularly
• Abdominal palpation
• Vaginal examination to
assess the progress of
labour (will always be done
prior pain relief being given)
1st Stage
Advanced
Labour
(Transition)
• Cervix dilates from 8cm
to 10cm (fully dilated)
• The baby’s head is flexed
and deep in the pelvis
The uterus may make mild
pushing efforts
• Very strong contractions
lasting up to 90 seconds
(all encompassing and
powerful)
• Irritable
• May have urge to push
at the height of each
contraction and you may
have anal pressure
• Nausea and vomiting are
common at this stage
• Listen to advice from the
midwife regarding the best
position to aid the descent
of your baby – all fours or
upright leaning forward
• Regular listening to baby’s
heartbeat
• The midwife will stay with
you during pushing and
encourage you both
2nd Stage
Pushing
• Cervix is fully dilated (10cm)
• Baby rotates in the pelvis,
trying to find the easiest
way out
• Gradually more of the
baby’s head becomes
visible. The head crowns
and is born
• With the next contraction
the shoulders and body
are born
• Urge to push
• May feel a burning
sensation as the perineum
stretches
• A sense of relief is generally
felt when the birth of your
baby is complete
• Get into a comfortable
pushing position
• Work with the urges, relax
all parts of your body
not directly involved with
pushing, particularly the
pelvic floor, mouth and
throat
• Push only with contractions
• The midwife will stay
with you
• The doctor will ease your
baby’s head out, and check
that the cord isn’t around
his/her neck
• The doctor will then
support the baby’s
shoulders and the rest of
your baby will be born and
placed on the mother’s
chest
3rd Stage
Delivery of
the Placenta
• Placenta separates from
the wall of the uterus
• Milder uterine contractions
• An intense interest in
your baby
• Push if asked to • The cord is then clamped
and cut, often by the father
or support person
• An injection of oxytocin is
given to the mother to help
the uterus contract and
separate the placenta